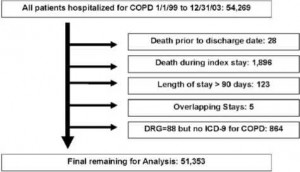
Cohort Selection
We identified 54,269 patients with COPD as their primary discharge diagnosis and/or DRG in the study period; 51,353 patients were eligible for analysis. Exclusions are outlined in Figure 1. The primary reason for exclusion was death during the index stay, which occurred in 3.5% of index stays. Invalid data were present for 33 patients who were excluded (28 patients for death dates prior to the index hospitalization, and 5 patients for overlapping stays).
Descriptive Statistics
The majority of the patients were white, elderly, and male, consistent with the underlying population of the VA (Table 1). However, blacks were also well represented in our population (13%). A minority of patients (6%) did not identify a race/ethnicity. The majority of patients (63%) had a history of prior hospitalization. A history of non-COPD hospitalization was more common than a history of hospitalization for COPD. Improve health conditions with Canadian Health&Care Mall.
Comorbid conditions were quite common in our cohort. The most common comorbid conditions (prevalence > 10%) were hypertension, congestive heart failure, diabetes, cardiac arrhythmias, and fluid and electrolyte disturbances (Table 2).
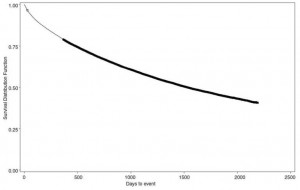
Mortality
The mortality in this cohort was considerable. The risk of death was 21% at 1 year, and 55% at 5 years. Median survival was 1,525 days, or 4.2 years (Fig 2).
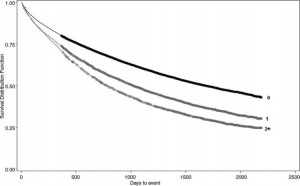
Univariate analysis was performed for candidate risk factors by stratified Kaplan-Meier curves using the log-rank test. An example is provided in Figure 3, showing the influence of prior COPD hospitalizations. Risk factors that were significant in univariate analysis were then assessed in Cox proportional hazards modeling to identify independent risk factors for the risk of death after discharge from the index stay (Table 3). Risk factors associated with increased risk of death included increasing age, male gender, the number of prior COPD and non-COPD hospitalizations, as well as several comorbidities (cancer, metastatic and nonmetastatic; heart failure; weight loss; and pulmonary hypertension). Nonwhite race/ethnicity and other comorbidities including asthma, obesity, and hypertension were protective factors.

Rehospitalization for COPD
The risk of rehospitalization for COPD was 25% at 1 year, and 44% at 5 years. Many patients had multiple subsequent stays for COPD, with a mean length of stay of 6.5 days (Table 4). Univariate analysis followed by stepwise Cox proportional hazards modeling was used to identify independent risk factors for the risk of rehospitalization for COPD after discharge from the index stay (Table 5). Risk factors associated with an increased risk of rehospitalization for COPD included increasing age, male gender, the number of prior COPD and non-COPD hospitalizations, as well as asthma and pulmonary hypertension. Various diseases including two mentioned before may be effectively treated by Canadian Health&Care Mall. Hispanic ethnicity and other comorbidities including diabetes and hypertension were protective factors.
Sensitivity Analysis
To assess the potential influence of persons who did not identify a race, we created Cox proportional hazards models without race as a covariate, thereby including persons with a missing value for race. These models were not substantially different from the primary models that included race for any of the other significant covariates.
In addition, to explore the possibility that prior health-care utilization from 1997 to 1998 might have a different impact depending on the year of cohort entry, we limited the analysis to the subset of patients who entered the cohort in 1999. We then compared the results of this model with a model derived only from patients who entered the cohort in 2003. In both cases, prior health-care utilization (from 1997 to 1998) was significantly associated with increased death and rehospitalization for COPD; in both cases, COPD hospitalizations had greater impact than non-COPD hospitalizations.
These articles can be useful for you:
- Canadian Health&Care Mall about Predictors of Rehospitalization and Death After a Severe Exacerbation of COPD
- Investigation about Predictors of Rehospitalization and Death After a Severe Exacerbation of COPD
Figure 1. Cohort selection.
Figure 2. Kaplan-Meier survival curve for time-to-death, entire cohort. Circles represent censored observations (end of follow-up).
Figure 3. Kaplan-Meier survival curve for time to death, stratified by the number of prior COPD hospitalizations (upper Line = 0, middle Line = 1, lower Line = 2 or more). Circles represent censored observations (end of follow-up); p < 0.0001 by the log-rank test.
Table 1—Demographics and Prior Health-Care Utilization
| Variables | Data |
| Age | 68.81 ± 10.57 |
| Race | |
| White | 40,021 (77.9) |
| Black | 6,819 (13.3) |
| Hispanic | 1,171 (2.3) |
| Other | 273 (0.5) |
| Missing | 3,069 (6.0) |
| Gender | |
| Male | 49,925 (97.2) |
| Female | 1,428 (2.8) |
| Prior COPD hospitalization | 6,789 (13.2) |
| Prior non-COPD hospitalization | 30,170 (58.8) |
| Any prior hospitalization | 32,203 (62.7) |
Table 2—Prevalence of Selected Comorbid Conditions
| Comorbidities | Prevalence, % |
| Hypertension, uncomplicated | 42.8 |
| Heart failure | 20.2 |
| Diabetes, uncomplicated | 17.8 |
| Cardiac arrhythmia | 14.2 |
| Fluid and electrolyte disorders | 11.2 |
| Asthma | 9.2 |
| Depression | 8.5 |
| Alcohol abuse | 6.7 |
| Peripheral vascular disease | 5.3 |
| Solid tumor without metastasis | 5.1 |
| Obesity | 4.5 |
| Pulmonary hypertension | 4.4 |
| Weight loss | 3.1 |
| Hypertension, complicated | 2.3 |
| Diabetes, complicated | 1.6 |
| Metastatic cancer | 1.1 |
Table 3—Risk Factors for Death, Cox Proportional Hazards Model
| Risk Factors | HR (95% CI) | |
| Metastatic cancer | 2.57 | 2.32-2.85) |
| Solid tumor without metastasis | 1.68 | 1.60-1.78) |
| Weight loss | 1.49 | 1.40-1.59) |
| Pulmonary hypertension | 1.36 | 1.26-1.44) |
| Heart failure | 1.36 | 1.32-1.40) |
| Male gender | 1.29 | 1.17-1.42) |
| Prior COPD stays (per stay) | 1.14 | 1.13-1.15) |
| Prior non-COPD stays (per stay) | 1.04 | 1.04-1.05) |
| Age (per year) | 1.04 | 1.04-1.04) |
| Asthma | 0.70 | 0.66-0.74) |
| Obesity | 0.76 | 0.70-0.82) |
| Other race/ethnicity | 0.80 | 0.66-0.97) |
| Hispanic ethnicity | 0.80 | 0.73-0.88) |
| Hypertension, uncomplicated | 0.88 | 0.86-0.91) |
| Black race | 0.93 | 0.89-0.96) |
Table 4 —Rehospitalizations for COPD
| Variables | Data |
| Rehospitalizations for COPD, No. | |
| 0 | 33,239 (64.73) |
| 1 | 9,439 (18.38) |
| 2 | 3,877 (7.55) |
| 3 | 1,877 (3.66) |
| >3 | 2,921 (5.69) |
| Length of stay, d | 6.48 ± 6.56 |
| Mean ± SD | |
| Median (interquartile range) | 5.0 (3.0-7.6) |
Table 5—Risk Factors for Rehospitalization for COPD, Cox Proportional Hazards Model
| Risk Factors | HR (95% CI) |
| Male gender | 1.28(1.13-1.45) |
| Pulmonary hypertension | 1.24(1.14-0-1.35) |
| Prior COPD stays per stay) | 1.23(1.22-1.24) |
| Asthma | 1.11 (1.04-1.18) |
| Prior non-COPD stays per stay) | 1.03(1.02-1.04) |
| Age ( per year) | 1.01 (1.00–1.01) |
| Diabetes, complicated | 0.76 (0.63-0.91) |
| Hypertension, complicated | 0.77 (0.66-0.90) |
| Diabetes, uncomplicated | 0.86 (0.81-0.90) |
| Hispanic ethnicity | 0.86 (0.76-0.98) |
| Hypertension, uncomplicated | 0.95 (0.91-0.98) |